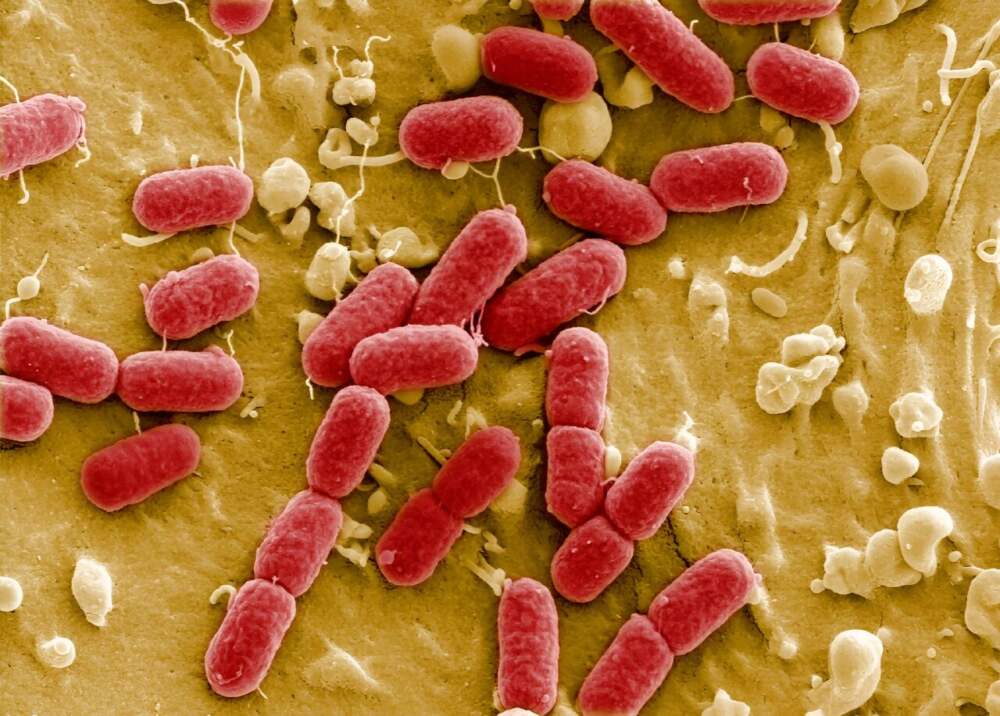
Health officials around the world are sounding a stark warning: antibiotic resistance has reached an alarming new level. According to the World Health Organization (WHO), one in six bacterial infections globally no longer responds to standard antibiotics — a figure that highlights a crisis decades in the making.
These so-called “superbugs” are spreading faster than previously anticipated, turning once-treatable illnesses into life-threatening conditions. What began as isolated hospital outbreaks has now evolved into a widespread global health emergency, threatening to undermine the very foundation of modern medicine.
A Global Health Crisis Unfolding
The WHO’s latest global report paints a grim picture of accelerating resistance across nearly every major bacterial strain tracked. Some regions, particularly in Asia, Africa, and Latin America, are seeing resistance rates soar to unprecedented levels. In parts of South Asia, for instance, nearly one-third of bloodstream infections are now resistant to frontline antibiotics such as carbapenems and cephalosporins — drugs once considered last-resort treatments.
In sub-Saharan Africa, the situation is even more dire. Bacteria that cause pneumonia, sepsis, and urinary tract infections are showing resistance levels above 70% in some countries. Even in high-income nations with robust healthcare systems, resistant infections are becoming more common in hospitals and long-term care facilities.
The result is a growing list of medical procedures — from organ transplants to chemotherapy — that carry increasing risk. Without reliable antibiotics, even minor surgeries or routine infections could become deadly.
Why Superbugs Are Rising
The rise of drug-resistant bacteria is not a sudden phenomenon. It is the predictable consequence of decades of overuse, misuse, and neglect.
- Overprescription: Antibiotics are frequently prescribed for viral infections like the common cold, against which they have no effect.
- Incomplete treatments: Patients often stop taking antibiotics once they feel better, leaving some bacteria alive to develop resistance.
- Agricultural misuse: Massive quantities of antibiotics are used in livestock to promote growth and prevent disease, creating a breeding ground for resistant bacteria that can spread to humans through food and the environment.
- Global inequality: Many developing countries lack proper healthcare infrastructure and diagnostic tools, making it difficult to track and control resistance.
- Stalled innovation: In the last three decades, only a handful of new antibiotics have been developed. Pharmaceutical companies often avoid antibiotic research due to high costs and low profitability.
These combined factors have created what experts call a “perfect storm” — an environment in which bacteria evolve faster than science can keep up.
The Human and Economic Toll
The consequences are devastating. The WHO estimates that antibiotic-resistant infections already cause more than a million deaths every year, with projections suggesting this number could rise to 10 million annually by 2050 if urgent action is not taken.
Beyond the tragic loss of life, the economic impact is enormous. Resistant infections lead to longer hospital stays, higher medical costs, and reduced workforce productivity. Developing nations, where surveillance and healthcare systems are weaker, bear the greatest burden — both in human suffering and economic strain.
Inside the Battle Against Resistance
Efforts to combat antibiotic resistance are underway, but progress remains uneven. Public health agencies worldwide are working to strengthen “antimicrobial stewardship” programs — initiatives that ensure antibiotics are used responsibly and only when necessary.
Hospitals are being urged to tighten infection control measures, while governments are investing in surveillance systems to track outbreaks more effectively. Researchers are exploring new frontiers in drug discovery, including phage therapy, AI-driven antibiotic development, and synthetic biology, which could lead to the next generation of antibacterial treatments.
However, experts warn that these efforts will only succeed if supported by global coordination and sustained political will. Resistance knows no borders — a superbug emerging in one country can quickly travel across continents through trade, travel, and migration.
Preventing the Post-Antibiotic Era
The WHO’s message is clear: humanity must act now to preserve the effectiveness of existing antibiotics while developing new ones. Some key steps include:
- Reducing unnecessary prescriptions by improving diagnostic tools and physician training.
- Investing in new antibiotics and alternative treatments to outpace bacterial evolution.
- Restricting antibiotic use in agriculture, replacing it with safer, sustainable practices.
- Enhancing global monitoring systems to detect and respond to resistant outbreaks quickly.
- Educating the public about the dangers of misuse and the importance of completing prescribed treatments.
Without immediate, coordinated action, the world could soon face a future where common infections are once again untreatable, and medical progress is set back by a century.
The Urgency of Now
The rise of superbugs is not a distant threat — it is happening today. From hospitals in major cities to rural clinics, doctors are encountering infections that no longer respond to available drugs. The implications are profound: if antibiotics lose their power entirely, modern medicine as we know it — including cancer care, surgery, and childbirth — could become perilous.
The WHO has declared antimicrobial resistance one of the top global health threats of the 21st century. Combating it will require a united effort that bridges science, policy, industry, and everyday behavior.
Antibiotics revolutionized healthcare in the 20th century. Now, protecting them may determine the future of medicine in the 21st.













Leave a Reply