Emerging research suggests that the shingles vaccine, widely used to prevent shingles (herpes zoster) in older adults, may also provide an unexpected benefit: reducing the risk of developing dementia. Large-scale observational studies conducted over the past decade indicate that adults who receive the shingles vaccine show a significantly lower incidence of cognitive decline compared with those who do not get vaccinated.
One notable study tracked more than 280,000 older adults over seven years. Researchers found that individuals who had received the shingles vaccine had approximately a 20% lower risk of being diagnosed with dementia. Other analyses corroborate these findings, showing reductions in dementia risk ranging from 17% to 33%, depending on the type of vaccine and the length of follow-up.
How the Shingles Vaccine Might Protect the Brain
The biological mechanisms behind this protective effect are not yet fully understood, but scientists propose several plausible explanations:
- Prevention of Viral Reactivation
After a chickenpox infection, the varicella-zoster virus remains dormant in nerve cells. Later in life, it can reactivate as shingles. This reactivation may trigger inflammation in the nervous system, which could contribute to cognitive decline. By preventing shingles, the vaccine may reduce these inflammatory episodes, indirectly protecting brain health. - Immune System Modulation
Vaccines stimulate the immune system, sometimes providing broader protective effects beyond the targeted disease. In the case of shingles vaccination, this immune activation may help reduce systemic inflammation, a factor linked to dementia and other age-related cognitive issues.
Evidence and Research Limitations
While the findings are promising, several caveats apply:
- Observational Nature: Most data come from observational studies rather than randomized clinical trials. While a strong association exists, causality has not been definitively established.
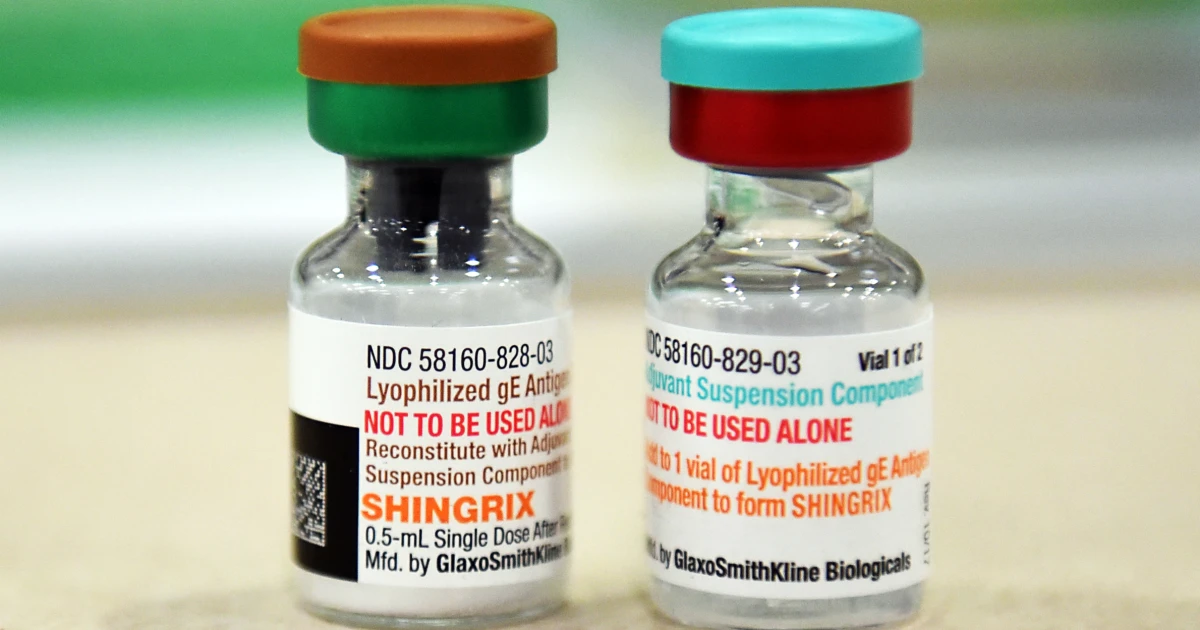
- Vaccine Variants: Different shingles vaccines (live attenuated vs. recombinant) may have varying effects on dementia risk, and research is ongoing to clarify these differences.
- Lifestyle Factors: Individuals who receive vaccines may also engage in other health-promoting behaviors—like regular exercise, healthy diet, and better medical care—that could independently lower dementia risk.
- Sex Differences: Some analyses suggest that women may derive more cognitive benefit from the shingles vaccine than men, though the reasons are still unclear.
Implications for Public Health
The potential cognitive benefits of the shingles vaccine have important implications:
- Encouraging Vaccination: Older adults eligible for the shingles vaccine now have an additional incentive beyond preventing painful shingles outbreaks.
- Complementing Other Interventions: While vaccination may help reduce dementia risk, it should be combined with established preventive strategies, including maintaining cardiovascular health, managing blood pressure, regular physical activity, mental stimulation, and social engagement.
- Guidance for Clinicians: Physicians may consider discussing the potential cognitive benefits when recommending shingles vaccination, particularly for patients at higher risk of dementia.
Broader Context
Dementia remains a major global health challenge, affecting tens of millions worldwide and placing significant social and economic burdens on families and healthcare systems. Interventions that even modestly reduce risk could have meaningful population-level benefits.
Vaccination as a dementia prevention strategy is part of a growing field investigating how immune modulation and infection control influence long-term brain health. Other vaccines, including influenza and pneumococcal vaccines, are also being studied for potential protective effects against cognitive decline.
Future Research Directions
Researchers aim to clarify several key questions:
- Which shingles vaccine types confer the strongest cognitive protection?
- How long does the potential protective effect last, and when should vaccination be administered for maximum benefit?
- What biological mechanisms underlie the link between vaccination and reduced dementia risk?
- Are there specific populations (e.g., by age, sex, or genetic predisposition) that benefit more from vaccination?
Long-term randomized trials and mechanistic studies are needed to address these questions and to determine how vaccination strategies might be integrated into broader dementia prevention programs.
Conclusion
The discovery that shingles vaccination may reduce the risk of dementia represents an exciting development in preventive medicine. While the vaccine should not replace other well-established strategies for brain health, it adds another tool to the growing arsenal of interventions aimed at preserving cognitive function in aging populations. For older adults, getting vaccinated against shingles may not only prevent painful outbreaks but also offer long-term benefits for the brain.














Leave a Reply