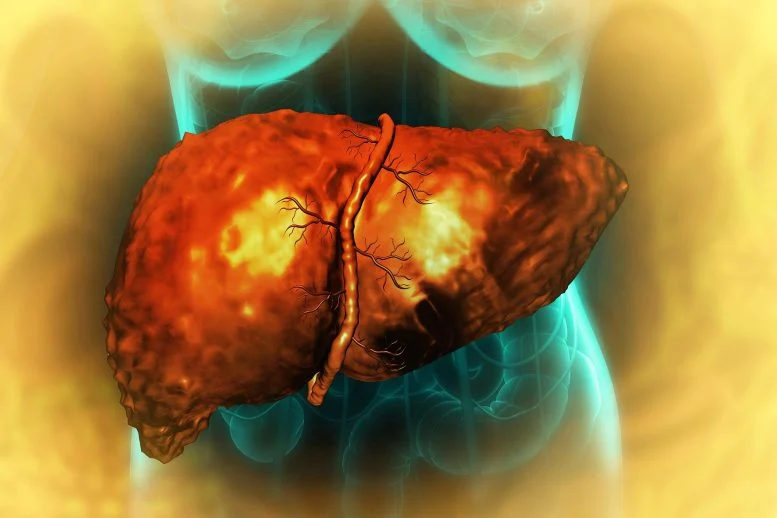
A groundbreaking study from the Massachusetts Institute of Technology (MIT) has unveiled how high-fat diets can silently predispose the liver to cancer, shedding new light on the molecular mechanisms linking diet, metabolic health, and cancer risk. The research provides compelling evidence that dietary choices have profound effects on liver biology, even before any outward signs of disease appear.
The study, conducted by MIT’s Department of Biological Engineering, investigated the effects of prolonged high-fat consumption on liver tissue in animal models. Researchers found that diets rich in fat do more than cause obesity or fatty liver disease—they also alter the cellular environment of the liver in ways that make it more susceptible to cancerous transformation.
“High-fat diets appear to prime liver cells at a molecular level, creating a fertile ground for cancer to develop later in life,” said Dr. Elena Rodriguez, lead author of the study. “These changes are subtle and occur long before conventional symptoms emerge, which is why diet-related cancer risk can be overlooked until it’s too late.”
The team discovered that excess dietary fat triggers chronic low-grade inflammation in the liver, accompanied by alterations in gene expression that regulate cell growth and metabolism. Specifically, certain signaling pathways involved in cell proliferation and DNA repair become dysregulated, increasing the likelihood that cells will accumulate mutations and progress toward malignant states.
In addition to molecular changes, the study highlighted the role of lipid accumulation within liver cells. While fatty deposits were expected, researchers found that these lipids also interact with cellular organelles such as mitochondria, impairing energy metabolism and increasing oxidative stress. This dual effect—genetic signaling disruption combined with metabolic stress—creates an environment highly conducive to tumor development.
The findings have significant implications for public health, particularly in regions where high-fat diets are common and liver cancer rates are rising. Non-alcoholic fatty liver disease (NAFLD), which affects millions globally, is now understood not just as a metabolic condition but also as a potential precursor to hepatocellular carcinoma, the most common form of liver cancer.
Importantly, the MIT study suggests that dietary interventions can reverse or mitigate these molecular changes if implemented early. Reducing saturated fat intake, increasing consumption of vegetables, whole grains, and lean proteins, and maintaining regular physical activity can help restore healthy liver function and reduce cancer risk.
“This research underscores the hidden dangers of high-fat diets,” Dr. Rodriguez explained. “It’s not just about weight gain; it’s about how what we eat reshapes our organs at a cellular level, sometimes in ways we cannot see.”
The study also opens new avenues for therapeutic development. By understanding the molecular pathways that link fat accumulation to cancer susceptibility, scientists may be able to design drugs that counteract these effects, offering protection to individuals at high risk or those already experiencing early stages of fatty liver disease.
Experts in the field are hailing the MIT findings as a wake-up call for both researchers and the public. “We’ve long known that obesity and poor diet are risk factors for liver disease,” said Dr. Marcus Lee, a hepatology specialist not involved in the study. “This research provides a mechanistic explanation, showing exactly how fat primes liver cells for cancer. It’s a major step forward in understanding disease prevention.”
With liver cancer remaining one of the deadliest malignancies worldwide, the study highlights the importance of preventative strategies and early lifestyle interventions. While genetics play a role, the MIT research reinforces the idea that diet is a modifiable factor that can dramatically influence long-term liver health.
As the study gains attention, researchers hope it will spark broader awareness of how everyday dietary choices shape disease risk, encouraging individuals and health authorities to prioritize nutritional education and proactive lifestyle changes.














Leave a Reply