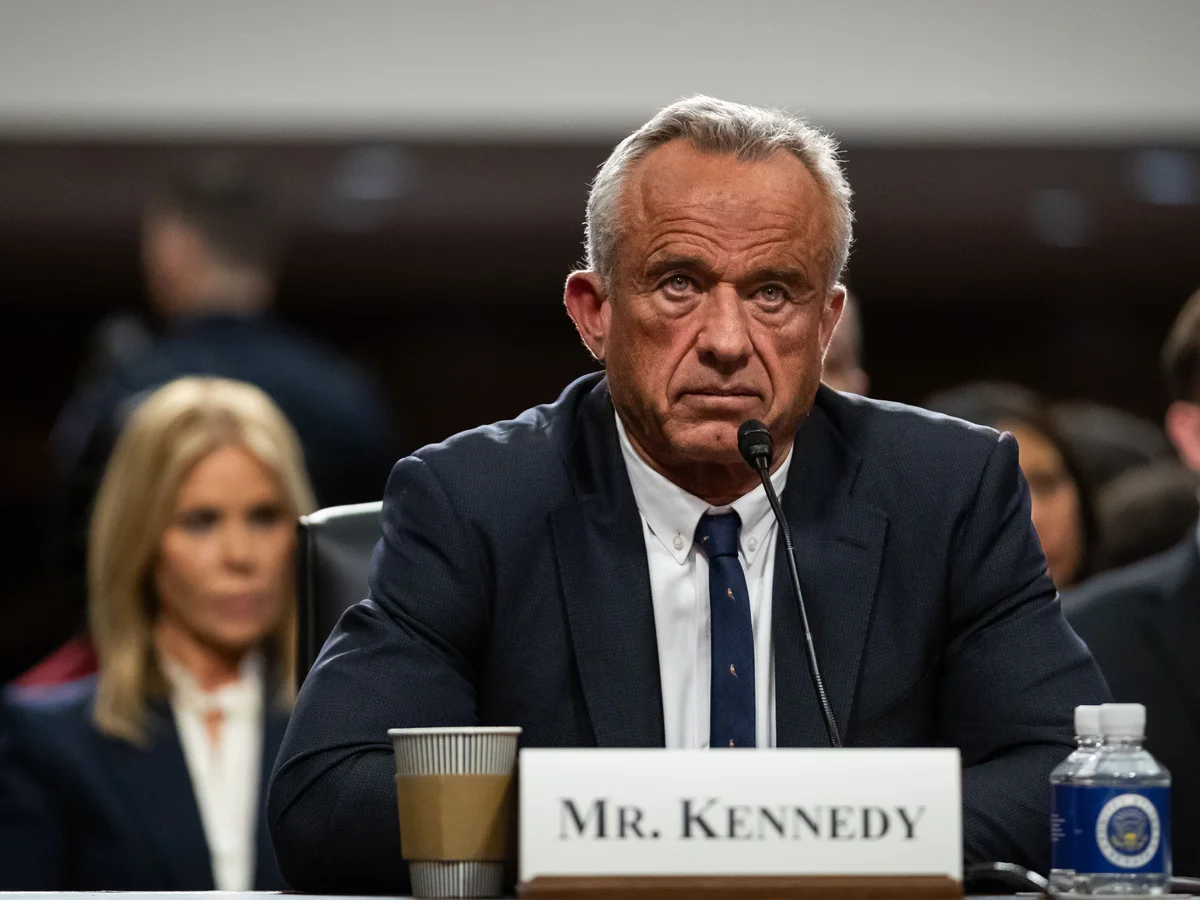
A controversial change in U.S. COVID-19 vaccine policy has put medical professionals at odds with political leadership. Dr. Pierre Kory, formerly affiliated with the University of Washington, has been dismissed and is now speaking out against updates to vaccine recommendations issued under Health Secretary Robert F. Kennedy Jr.
What’s Different in the New Guidance
- Under the updated framework, COVID-19 vaccine guidance will no longer carry broad recommendations for most Americans. Instead, vaccination is now promoted as an individual decision, to be made in consultation with a healthcare provider.
- The new policy places emphasis on evaluating risk. High-risk individuals—older adults or those with underlying health conditions—are still strongly advised to get vaccinated, while the general population is encouraged to consider benefits and risks.
Dr. Kory’s Position
- Dr. Kory argues that the new guidance under-cuts decades of public health practice, which relied on strong, uniform vaccine messaging to protect communities. He believes this shift could lead to lower uptake, poorer outcomes, and more confusion.
- He has criticized what he sees as political interference in scientific institutions. Kory says that changing vaccine messaging without clear, peer-reviewed evidence sets a dangerous precedent for policy driven by politics rather than medicine.
- In voicing his concerns, he warns of potential downstream effects: reduced coverage, increased vulnerability among populations less engaged with healthcare, and erosion of trust in public health.
Broader Context & Criticism
- The advisory committee behind the updated guidance was recently reconstituted by RFK Jr., replacing the previous panel with new appointees, some of whom have questioned aspects of vaccine science in the past.
- Former CDC officials and other public health experts express concern that the new committee members may be less steeped in vaccination science, potentially leading to guidance that emphasizes uncertainty more than data.
- Critics are also voicing worries about how insurance coverage, vaccine access, and public health programs might adapt to the new recommendation paradigm.
Implications for Public Health
- If fewer people are strongly encouraged to vaccinate (beyond high-risk groups), there could be reduced community protection, particularly in areas with low vaccination rates. Diseases spread more easily when uptake drops.
- Public messaging becomes more complex. Agencies will need to balance individual autonomy with encouraging vaccine confidence, especially among populations with limited access to healthcare or information.
- The change may affect how vaccine policies are implemented at state and local levels, including coverage by insurance plans and supply chain planning for vaccine distribution.
What to Watch
- How states and private health providers adjust their policies in response to the guidance: will they still promote COVID vaccination broadly, or scale back given the new tone?
- Whether the shift results in lower vaccination rates and, if so, whether we see increases in COVID-related hospitalizations or outbreaks among unvaccinated or undervaccinated communities.
- The ongoing debate among scientists, public health leaders, and policymakers about evidence standards, transparency, and the role of politics in health guidance.
- Legal or regulatory consequences tied to insurance reimbursements, vaccine mandates (where they exist), and vaccine access in public programs like those serving children.
Conclusion
The removal of a broad recommendation for COVID-19 vaccination in favor of individualized decision-making has ignited intense debate. Dr. Kory’s criticism highlights fears that changing course without a clear evidentiary consensus could weaken vaccination efforts and public trust. As policy shifts ripple through healthcare systems, the ultimate impact may show in how well Americans make informed choices—especially those most vulnerable.














Leave a Reply