A growing chorus of physicians is urging more awareness and updated guidance around mesenteric ischemia, a condition where blood flow to the intestines is reduced or blocked. Northwestern University doctors in particular have raised alarms that both acute and chronic forms are often underdiagnosed, leaving patients to suffer unnecessarily.
What Is Mesenteric Ischemia?
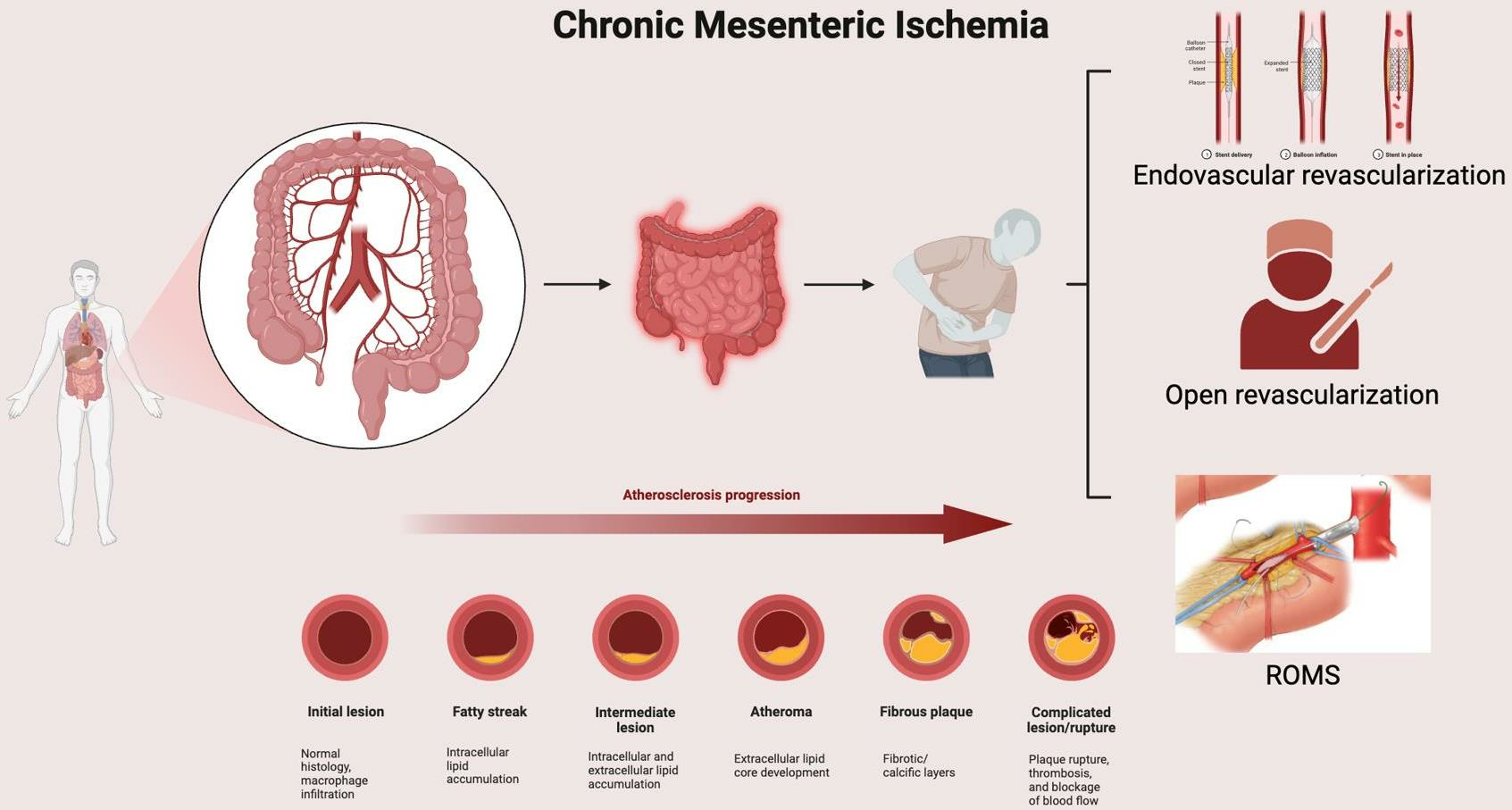
- The mesenteric arteries are the blood vessels that supply oxygen-rich blood to the intestines. Reduction or blockage in these arteries causes mesenteric ischemia.
- There are two main forms:
- Acute Mesenteric Ischemia – sudden blockage (often from a blood clot) that can cause severe abdominal pain, potentially life-threatening damage to intestines if not treated promptly.
- Chronic Mesenteric Ischemia (CMI) – develops gradually (often due to narrowing of the arteries from atherosclerosis) and leads to symptoms like pain after eating, unintentional weight loss, nausea, and fear of eating because it causes discomfort.
Why the Concern Now
- Doctors at Northwestern and elsewhere say CMI is often missed because its symptoms overlap with other gastrointestinal issues—gas, ulcers, gallbladder disease, or simply indigestion. Because of this, patients may go months or even years without an accurate diagnosis.
- Many patients with CMI are assumed to have non-serious digestive problems and are treated accordingly, delaying vascular evaluation and possible lifesaving intervention.
- Another complicating factor: not all patients presenting with symptoms fit the “classic” profile. While CMI is more common in older adults with risk factors like smoking, hypertension, high cholesterol, heart disease, or diabetes, younger or overweight patients may also suffer from it—even when they have none or few of those risk markers.
New Insights & Research Findings
- Researchers at Northwestern have contributed to recent studies showing that patients’ body mass index (BMI) plays a significant role in long-term outcomes after treatment of CMI. In particular, overweight status appears to influence survival after revascularization surgeries.
- Comparative studies between open surgery and less invasive endovascular approaches show that choice of procedure, patient health status (including kidney function, comorbidities), and how early the disease is caught all matter greatly for outcomes.
What Patients & Clinicians Should Watch For
- Symptoms to monitor: Pain after eating (post-prandial pain), unintended weight loss, chronic nausea or vomiting, fear of eating due to pain. These symptoms are sometimes dismissed or treated as more benign gastrointestinal problems.
- Risk factors: Smoking, heart disease, diabetes, high blood pressure, high cholesterol, older age, kidney disease. Also, history of clotting disorders.
- Diagnosis tools: Modern vascular imaging (such as CT angiography), ultrasound of mesenteric vessels, and sometimes diagnostic angiography help identify artery narrowing or blockages.
Treatment Options
- Lifestyle & Medical Management: Risk factor control is critical—quitting smoking, controlling blood pressure, managing lipids, ensuring good glycemic control in diabetics. Proper diet and weight management can make a difference.
- Revascularization Procedures: These can be done in two main ways:
- Open surgery (bypass grafts or arterial reconstruction)
- Endovascular techniques (angioplasty, stenting)
- The choice depends on how advanced the disease is, patient health, anatomy of the arteries, and presence of other medical issues.
Challenges & What’s Needed
- Delays in diagnosis remain a major hurdle. Because the disease is rare and symptoms overlap with more common conditions, doctors often wait before ordering the imaging studies that reveal vascular problems.
- Postoperative care and long-term follow-up are crucial but not always standardized, especially for chronic forms. Patients often require periodic imaging to ensure that vessels stay open, and close monitoring of nutrition and digestive function.
- More public and physician awareness is needed—many people do not know mesenteric ischemia exists, or that weight loss and eating avoidance may be red flags.
Bottom Line
Mesenteric ischemia may not be widely known, but it deserves more attention. For people experiencing pain after eating, unintended weight loss, and digestive symptoms without a clear cause, it should be considered. Early diagnosis, timely vascular evaluation, and appropriate treatment can dramatically improve outcomes—sometimes making the difference between ongoing suffering and restored quality of life.













Leave a Reply