September 24, 2025
A major U.S. vaccine advisory committee has recently made several adjustments to its guidance on COVID-19, MMRV (measles-mumps-rubella-chickenpox), and hepatitis B vaccines. These updates affect who is urged to get vaccinated, when, and under what circumstances. Here’s a breakdown of what changed and how you can still get these vaccines.
What’s Changed
- COVID-19 Vaccination Recommendations Shift
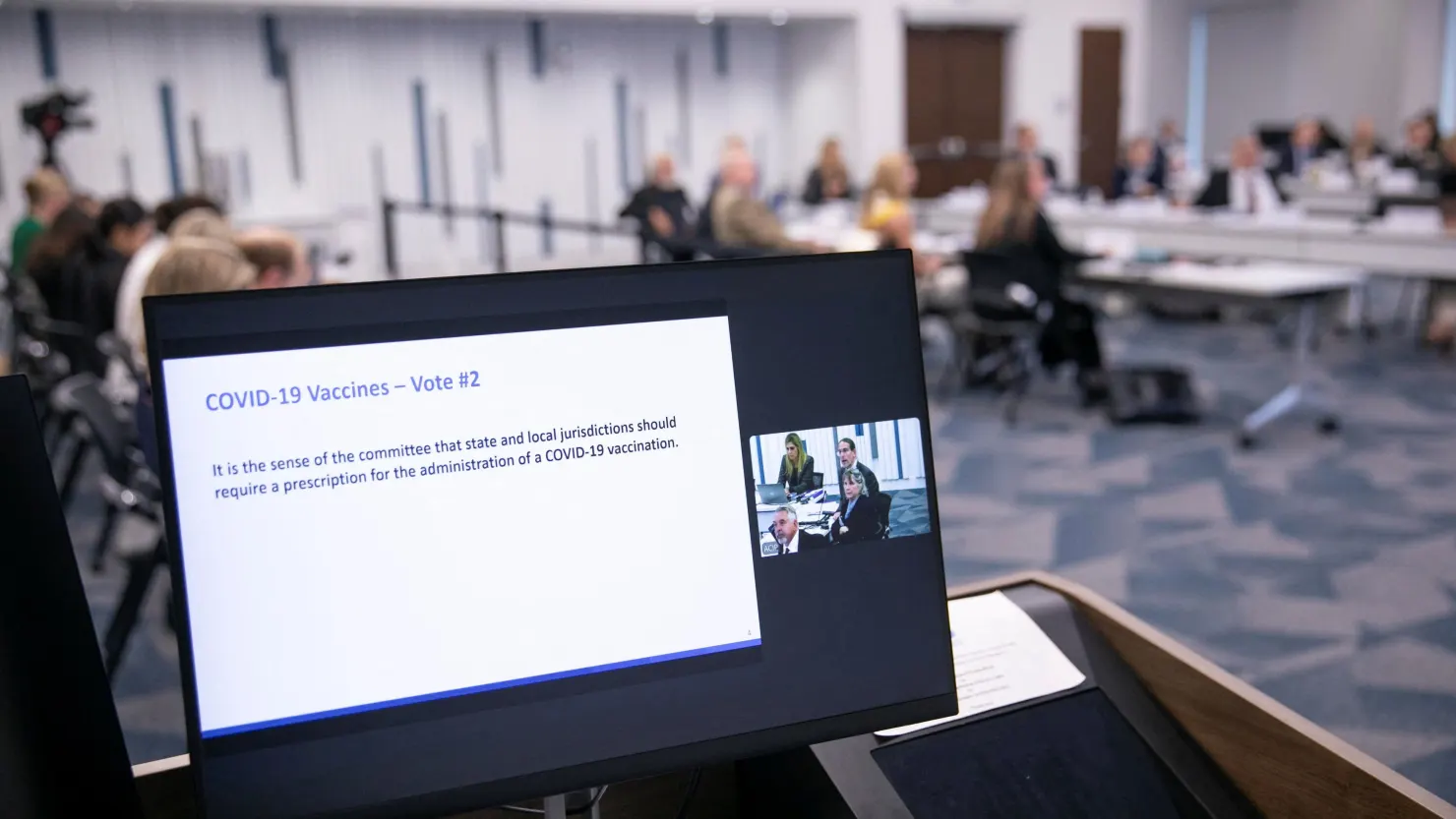
The advisory group no longer broadly recommends that everyone six months and older must get the COVID-19 vaccine each season. Instead, the decision is now framed as a shared, individual-clinical decision. This means people are encouraged to discuss with healthcare providers whether the vaccine makes sense for them based on their risk. The committee also decided not to require a prescription to receive the COVID-19 vaccine. - MMRV Vaccine (Measles, Mumps, Rubella, Varicella)
For children under age 4, the combined MMRV vaccine is no longer recommended. Health experts prefer that young children receive separate MMR and varicella (chickenpox) shots instead of the combined 4-in-1 vaccine. Part of this decision comes from a slightly higher risk of fever-related seizures when the combined vaccine is used in very young children. - Hepatitis B at Birth Questioned — For Now Unchanged
There was debate about whether to delay the first dose of hepatitis B vaccine for newborns in cases where mothers test negative for hepatitis B. However, no change was made: the current recommendation to give the first dose at birth remains in place. The committee did vote to increase testing of pregnant women for hepatitis B to ensure better prevention of mother-to-child transmission.
How to Get These Vaccines Under the New Guidance
Even with updated guidance, these vaccines remain accessible. Here’s how:
- If you’re eligible, talk to your primary care doctor or a pediatrician. They can offer personalized advice, especially for COVID-19, to figure out risk versus benefit.
- Clinics, community health centers, pharmacies, and public health departments still carry COVID-19 vaccines for people six months and older. If you qualify (age, health condition, pregnancy, etc.), you can receive them even though the messaging has changed to more individual decision-making.
- For children under age four, request the separate MMR + varicella vaccines instead of the combined MMRV shot. Most providers will follow the new guidance once official implementation happens.
- For newborns, the hepatitis B vaccine given at birth remains part of standard prenatal and newborn care protocols. Hospitals and birth centers should still routinely offer this.
What to Know Before You Go
- Insurance still tends to cover these vaccines, especially if your provider follows national guidance. Even with recommendation changes, publicly funded programs usually align with the advisory committee’s decisions.
- Ask about possible side effects. With COVID-19, vaccine side effects are generally mild, though risk-benefit depends more strongly on individual health risks now. With MMRV versus separate shots, the risk being discussed is mainly a higher rate of fever‐associated seizures in young children—though these events are rare and typically short-lived.
- For hepatitis B: catching and treating infections early is critical. Be sure that your or your child’s caregiver is informed about mother-to-child transmission if applicable.
Bottom Line
The recent vaccine guideline changes reflect a shift toward more personalized decision-making, especially for COVID-19, but they do not close the door on getting vaccinated. MMRV for young children is less favored, and hepatitis B remains standard at birth. If in doubt, a conversation with your healthcare provider will help clarify what’s best for you or your family.














Leave a Reply