September 24, 2025
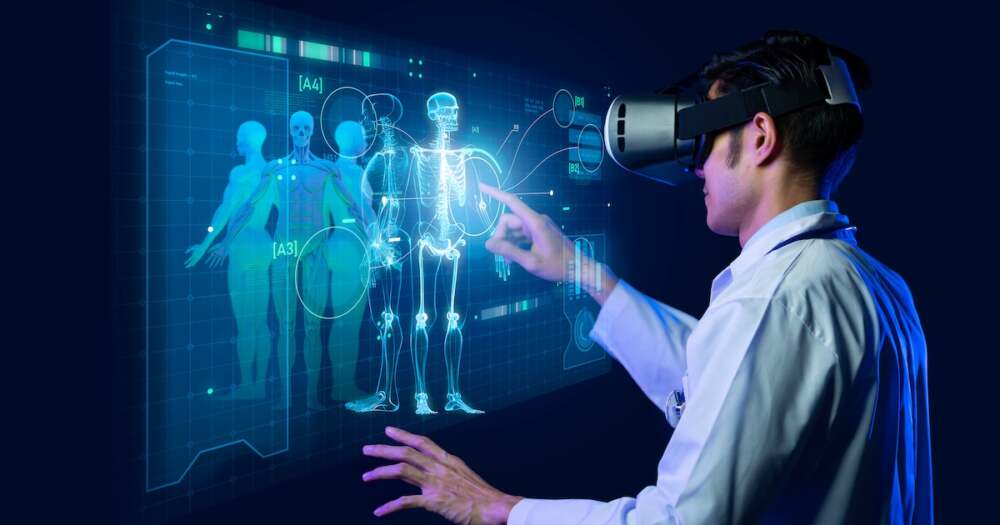
Health care decisions are undergoing a major shift as private insurers increasingly deploy artificial intelligence to decide whether to approve or deny patient care. Following this trend, Medicare is poised to launch its own AI-driven system for prior authorization — meaning many more medical decisions will soon be made, in part, by algorithms rather than humans.
What’s Happening
- Private insurers have already been using machine-assisted reviews to speed up prior authorization requests — those “permission checks” required before certain services, procedures, or medications can be covered. These systems examine medical records, billing codes, and even past claim outcomes to decide automatically whether care is “medically necessary.”
- Studies show that since adopting AI-based tools, some insurers have significantly increased denial rates, especially for post-acute care such as rehabilitation, long-term care, or other specialized services. In many cases, denials occur without direct human review, or with minimal oversight.
- Recognizing both the cost pressures and the controversy around private insurers’ use of AI, Medicare will soon begin testing its own prior authorization pilot program using similar AI tools. The move is framed as an attempt to speed up decision-making, reduce backlog, and perhaps cut unnecessary costs — but it comes with concerns.
Concerns and Risks
- Transparency and accountability: Critics argue insurance algorithms are often “black boxes” — patients and doctors may not know why a request was denied, what data the algorithm used, or how to challenge it.
- Human oversight: With automation comes risk of errors — wrong diagnosis matching, outdated protocols, or missing context that only a human clinician would catch. Doctors have raised alarms that many algorithmically-made denials are overturned on appeal, suggesting the systems may err on the side of denial to save costs.
- Patient harm: Delays or outright denial can jeopardize patient health, especially for those needing timely care such as therapies after surgery, cancer treatments, physical rehabilitation, or mental health services.
- Unequal impact: Vulnerable populations — the elderly, disabled, those with complex conditions — are especially likely to suffer because their cases can be more nuanced and may not fit neatly into algorithmic checklists.
How Patients & Providers Can Respond
- Patients can ask their doctors to challenge denials (submit appeals), provide full medical documentation, and insist on peer review or human-led reviews when available.
- Providers should stay informed about how their insurer uses AI tools, what rules apply, and what the appeal process looks like. Clear communication with patients about possible coverage issues is more important than ever.
- Advocacy and regulatory pressure are growing. Some health policy experts urge stricter rules: requiring insurers to explain AI decisions, ensuring a human clinician reviews complex cases, and setting safeguards so that cost savings don’t come at the expense of patient care.
What the Medicare Move Means
- If Medicare’s pilot program works efficiently, it could become the model for future public insurance benefit decisions — potentially speeding up approvals for many beneficiaries.
- On the other hand, it could expand the number of denials too if the AI tools are tuned to avoid financial risk rather than prioritize care. How well the program balances speed, fairness, safety, and human review will determine whether patients see benefit or harm.
- Policymakers and health regulators will be watching closely to see what oversight, transparency, and protections are included, particularly since the scale of Medicare is large and its decisions affect millions.
Bottom Line
AI in insurance prior authorizations is accelerating — private plans have led the way, and Medicare is about to join in. While there are promises of greater efficiency and lower cost, there are also serious concerns around fairness, patient rights, and the potential for harm. As health care decision-making becomes more automated, oversight, transparency, and appeals systems will be key to making sure care remains accessible and humane.













Leave a Reply