As the United States enters its fifth year of grappling with COVID-19, data from 2024 shows a modest decline in deaths from the virus. While the reduction marks progress, COVID-19 continues to rank among the top ten leading causes of death in the country, signaling that the pandemic’s impact is far from over.
Overview of 2024 Mortality Trends
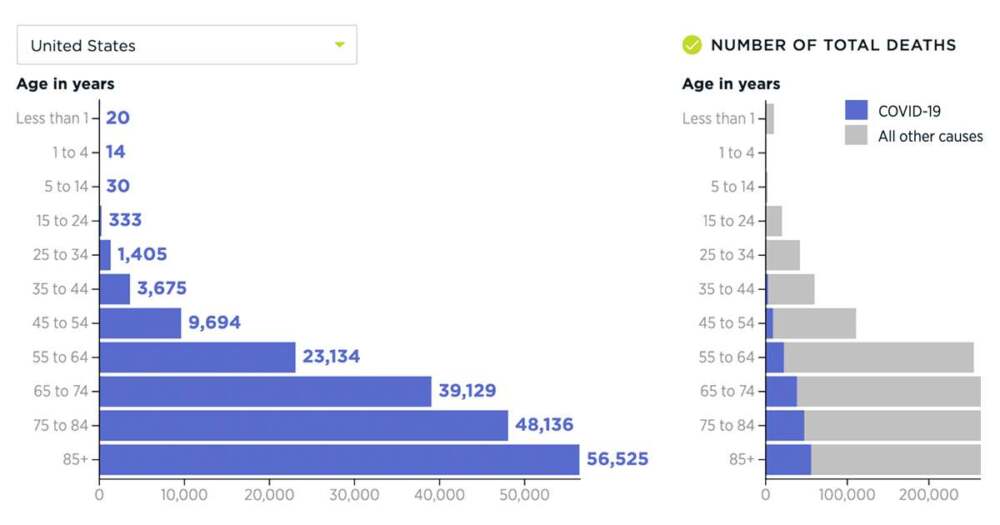
In 2024, approximately 100,000 Americans died from COVID-19, reflecting a decrease of about 6% compared to the previous year. Most fatalities were concentrated among adults aged 65 and older, highlighting the persistent vulnerability of older populations. Younger age groups experienced significantly fewer deaths, though hospitalizations and severe cases still occurred.
Despite widespread availability of vaccines and antiviral treatments, the virus maintained a steady toll due to uneven vaccine uptake, emergence of new variants, and ongoing strain on healthcare systems. Public health experts caution that while the trend is encouraging, complacency could reverse these gains.
Factors Contributing to Continued Mortality
- Vaccine Hesitancy and Gaps in Immunization
While vaccination rates in the U.S. improved over the years, many adults—especially in certain geographic regions and age groups—remained unvaccinated or did not receive booster doses. Public health officials note that even moderate vaccine coverage gaps can lead to preventable hospitalizations and deaths, particularly among those with underlying health conditions. - Emergence of New Variants
COVID-19 continues to evolve, with several new variants circulating in 2024. Some of these variants demonstrated increased transmissibility and partial resistance to immunity from prior infection or vaccination. Localized surges caused hospital overcrowding in some regions, stressing both acute and long-term care facilities. - Healthcare System Strain
Hospitals and clinics, particularly in rural or underserved areas, faced challenges maintaining staffing levels and resources. This strain sometimes resulted in delayed care, impacting both COVID-19 patients and those with other medical emergencies. - Comorbidities and Vulnerable Populations
Individuals with pre-existing health conditions—including diabetes, heart disease, obesity, and chronic respiratory illnesses—remained at higher risk of severe outcomes. Long-term care facilities continued to be hotspots for outbreaks, necessitating strict infection control measures.
Public Health Response and Strategies
Despite these challenges, public health authorities continued efforts to mitigate the impact of COVID-19 in 2024:
- Vaccination Campaigns: Targeted campaigns aimed to increase booster uptake, particularly among older adults and high-risk populations.
- Testing and Monitoring: Expanded testing and genomic surveillance helped identify outbreaks and track emerging variants more rapidly.
- Treatment Access: Widespread availability of antiviral medications and monoclonal antibody therapies helped reduce hospitalization and mortality in high-risk individuals.
- Public Awareness: Health agencies promoted mask-wearing in crowded or high-risk settings, alongside guidance for managing symptoms and seeking medical care promptly.
Experts note that ongoing vigilance is critical. While COVID-19 may no longer dominate headlines as it did in the early years of the pandemic, the virus continues to claim lives and requires sustained public health interventions.
Lessons and Looking Forward
The decline in death rates demonstrates the benefits of vaccination, therapeutics, and improved public health strategies. However, the persistence of tens of thousands of deaths each year underscores the need for continued investment in:
- Vaccine development to address evolving variants.
- Healthcare infrastructure to support pandemic response.
- Public health education to reduce misinformation and improve vaccine uptake.
Researchers emphasize that COVID-19 is likely to become endemic, meaning it will circulate in the population for the foreseeable future. Effective management will depend on maintaining high levels of immunity, quickly identifying outbreaks, and protecting the most vulnerable populations.
Conclusion
The United States has made progress in controlling COVID-19, but the virus remains a serious public health concern. With ongoing vaccination, monitoring, and preparedness efforts, further reductions in mortality are possible. Yet, experts warn that the virus is not yet behind us, and sustained vigilance is essential to protect communities and prevent future surges.










Leave a Reply