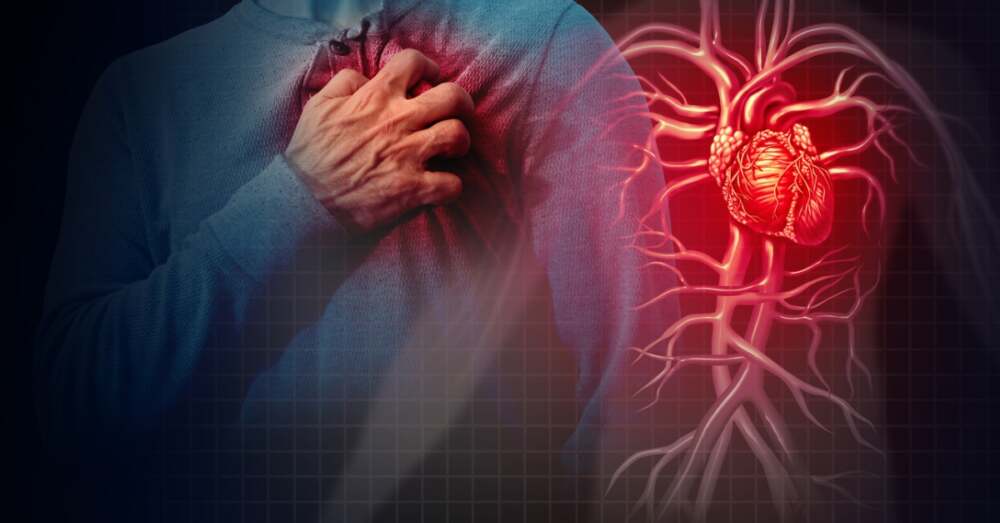
Heart disease continues to sit at the top of global health threats, often striking without warning and disproportionately affecting those with hidden or underestimated risk factors. Despite advances in medicine, many people remain unaware of what truly puts them in danger—and how much control they might have over it.
Unseen Culprits: Beyond Just Cholesterol and Blood Pressure
When most people think of heart disease, they picture clogged arteries, high blood pressure, or high cholesterol. While these are key players, researchers are increasingly spotlighting less obvious, but equally important factors:
- Genetic markers and “silent” lipoproteins: Certain inherited markers—like elevated levels of Lipoprotein(a)—don’t show symptoms until damage accumulates. Some cardiologists are now recommending that people, especially those with family history, get tested for these hidden risk factors.
- Chronic inflammation, oxidative stress, and metabolic dysfunction: Diets high in processed foods, environmental pollutants, sedentary life, and metabolic disorders (e.g. insulin resistance) can quietly erode cardiovascular health over years.
- Sleep health and stress: Repeated nights of poor sleep or high stress levels raise blood pressure, disrupt heart rhythms, and aggravate inflammation.
- Hormonal shifts and gender-specific risks: For women, hormonal changes (e.g. menopause) can accelerate plaque buildup or destabilize vascular health. Some heart attack causes in younger women (e.g. spontaneous coronary artery dissection) deviate from the classic pattern of atherosclerotic blockages.
- Lifestyle overlaps: Smoking, excessive alcohol, obesity, inactivity, and diets high in sugar or trans fats still carry heavy weight—but their interplay with lesser-known risks is what amplifies danger.
Why Many Heart Attacks Come “Out of the Blue”
One of the most alarming aspects of heart disease is that many first cardiac events come as a sudden shock. Some contributing reasons:
- Risk factors accumulate silently: Changes in arteries, small blockages, and vessel wall damage build gradually. Often no noticeable symptoms arise until something triggers a blockage or rupture.
- Individual variation: Two people with similar cholesterol or blood pressure can have dramatically different outcomes depending on genetics, inflammation levels, or how their body handles oxidative stress.
- Misdiagnosis or overlooked signs: Symptoms like fatigue, shortness of breath, or mild chest discomfort are often dismissed or attributed to less serious causes.
- Nontraditional causes: Some heart attacks, especially in younger individuals or women, are due to causes other than clogged arteries—like embolisms, arterial dissection, or microvascular disease.
What You Can Do to Tip the Balance in Your Favor
Fortunately, while some risk factors are beyond control, many are well within reach. Here’s by what you can take charge:
| Strategy | Why It Matters | Action Steps |
|---|---|---|
| Get a full cardiovascular workup | Basic tests (cholesterol, blood pressure) may miss “silent” risks | Ask your doctor about tests for Lipoprotein(a), CRP, advanced lipid panels |
| Adopt a heart-healthy diet | Helps maintain vascular health, control inflammation | Emphasize whole grains, veggies, lean proteins, healthy fats; reduce processed foods |
| Exercise consistently | Strengthens the heart, improves circulation, lowers risk | Aim for ≥150 minutes/week of moderate activity, plus strength training |
| Focus on sleep & stress | Restorative sleep and lower stress reduce strain on your cardiovascular system | Prioritize 7–9 hours sleep, practice stress management (meditation, hobbies) |
| Avoid tobacco & limit alcohol | Smoking and excess drinking damage vessels and promote plaque | Quit smoking, limit alcohol to moderate intake |
| Stay vigilant with symptoms | Catching warning signs early can prevent full cardiac events | Don’t dismiss fatigue, chest discomfort, shortness of breath, or irregular heartbeat—see a doctor |
What This Means for Your Health Journey
Understanding heart disease as a multifaceted, layered risk helps shift the narrative from “inevitable aging” to “manageable health.” It’s no longer enough to focus only on cholesterol or blood pressure—holistic approaches that encompass genetics, lifestyle, environment, and preventive screening offer the greatest protection.
For your readers: encourage them to ask their doctors tough questions, push for comprehensive testing (not just basic panels), and adopt preventive strategies early—before symptoms emerge. In many cases, it’s the quiet changes we apply every day that make the difference.













Leave a Reply