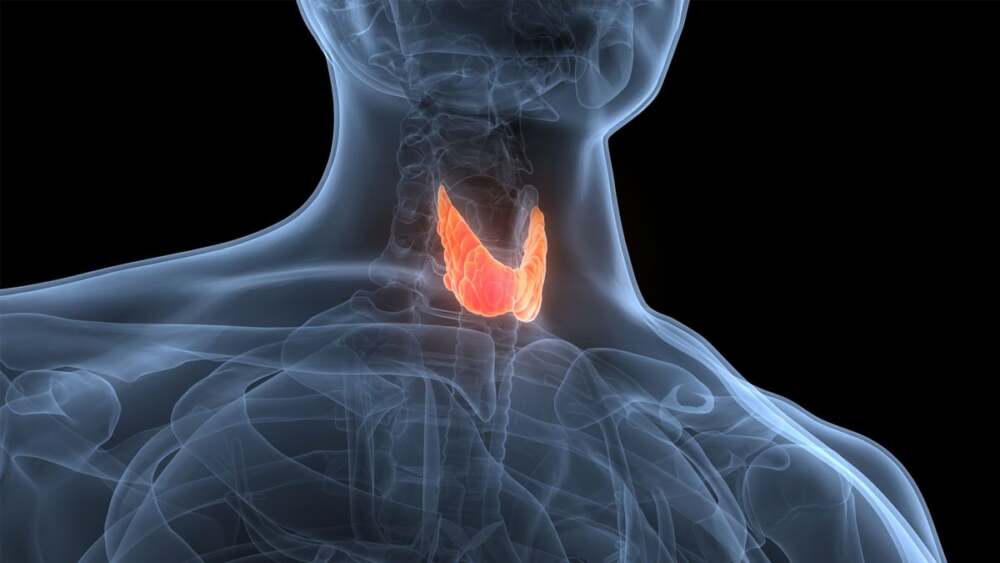
There is growing concern among doctors that widely used thyroid investigations could be leading to unnecessary fear, treatment, and expense due to overdiagnosis of thyroid cancer. While early detection is widely viewed as a medical good, the nuance is that not all abnormalities found in the thyroid pose a real threat—but many are treated as though they do.
What’s the Issue
A large number of people undergo thyroid screening or imaging (via ultrasound or other scans) for various reasons—sometimes unrelated to thyroid disease. These tests often reveal nodules (small lumps) in the thyroid gland.
Most of those nodules are benign (non-cancerous). In fact, studies show that over 90% of thyroid nodules never become serious or cause harm.
However, once a nodule is found, there tends to be pressure (from both patients and medical practice norms) to get more tests, biopsies, or even go ahead with surgical removal of part or all of the thyroid. Sometimes this happens even when indicators suggest the risk of malignancy is low.
Why Overdiagnosis Happens
Imaging sensitivity: Modern imaging techniques are very good at finding tiny nodules, many of which would never grow or cause symptoms. But detecting them increases the chance of a cascade of interventions.
Risk aversion: Both doctors and patients often prefer to act early rather than risk missing a cancer diagnosis—even when the risk is small.
Uncertain diagnostic categorization: Some biopsies yield results that are ambiguous—neither clearly benign nor clearly malignant. When results are “indeterminate,” the default response in many settings is to lean toward surgery.
Medical guidelines and norms: In many health systems, standard protocols or legal liability fears push toward treating found nodules aggressively.
Consequences of Treating Too Much
Unnecessary surgery: Removing thyroid tissue when it may not have been needed can bring risks—surgical complications, lifelong hormone replacement, impacts on calcium metabolism, and sometimes damage to the voice or swallowing functions.
Psychological burden: Being diagnosed with something called “cancer” or a “pre-cancerous lesion” can cause significant anxiety, even when the risk is minimal.
Burden on healthcare resources: Unnecessary tests, follow-ups, surgeries, and long-term medication use cost both individuals and health systems.
What Doctors Propose as Possible Fixes
More selective screening: Rather than broadly applying imaging or ultrasound tests in people without symptoms, some experts recommend reserving them for higher-risk cases (family history, exposure to radiation, etc.).
Better diagnostic tools: Molecular testing or newer biomarkers can sometimes help distinguish which nodules are more likely to turn malignant, reducing ambivalence in biopsy results.
Active surveillance: For small, low-risk nodules, closely monitoring without immediate surgery is increasingly accepted as a safe option in many cases.
Clearer guidelines and patient education: Ensuring that patients understand the risks, benefits, and uncertainties of treatment vs observation helps in making more balanced decisions.
Bottom Line
While thyroid tests and imaging have undoubtedly saved lives by catching cancers early, there is a tipping point where benefit turns into harm. Doctors fear that the current level of detection—especially of small, low-risk nodules—is pushing many people toward invasive treatments that may not improve long-term outcomes. The challenge going forward is to find the balance: detecting serious disease early, but avoiding overdiagnosis and overtreatment.













Leave a Reply